Introduction:
Understanding decisional involvement and information preferences in patients with hematologic malignancies may help to optimize physician-patient communication about treatment decisions and align the decision-making processes with patients' preferences. Exploring how patients perceive their length of life compared to an average person (prognostic optimism) may allow tailoring of conversations about treatment and prognosis. We described and examined factors associated with decisional involvement preferences, information preference, and prognostic optimism.
Methods:
In a multicenter observational study, we recruited patients with hematologic malignancies of any stage from 9/2003 to 6/2007. Patients were asked about: 1) Decisional involvement preference (Control Preferences Scale), 2) Information sources (including most useful source of information), 3) Preferences for types of information, 4) Preferences for presentation of treatment success information by their oncologists, and 5) Self-perceived length of life compared to patient estimates of an average person of the same disease type and stage (0-6 months, 6-12 months, 1-3 years, 3-5 years, 5-10 years, and >10 years); prognostic optimism was defined as present if patients perceived that they would live longer than their estimates of an average person with the same disease type and stage. We used multivariate logistic regressions to determine demographic and clinical factors associated with: 1) Decisional involvement preference, 2) Usefulness of information sources, and 3) Prognostic optimism.
Results:
Among 216 patients, median age was 55 years (range 22-79); 39% had lymphoma, 19% had acute leukemia, and 13% had multiple myeloma.
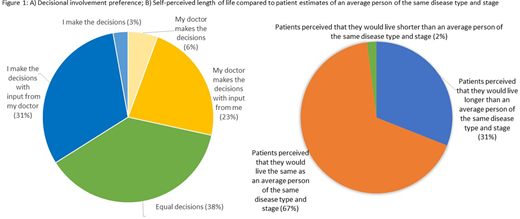
In terms of decisional involvement preferences, patient-directed, shared, and physician-directed approaches were preferred in 34%, 38%, and 28% of patients, respectively (Figure 1a). On multivariate analysis, none of the demographics or clinical factors were associated with decisional involvement preferences.
Common sources for patients to obtain information on disease or treatment options included their physician (98%), computer/internet (87%), print and broadcast media (71%), and family/friends/other patients/patient support group (78%). Utilization of computer/internet was higher among patients aged <60 years compared to those ³60 years (91.2% vs. 80.5%, P=0.02).. On multivariate analysis, patients with less than a college education (vs. postgraduate education) were less likely to perceive their physician as the most useful source [Adjusted Odds Ratio (OR) 0.46, p=0.05]. Patients with acute leukemia were more likely to perceive their physician as the most useful source (OR 2.49, p=0.03) compared to patients with other blood cancer
Over 90% of participants indicated that they would like to discuss each of the following disease and treatment issues: treatment options, goals, impact of disease and treatment on lifestyle, likelihood of treatment success, average survival, physician recommendations for treatment, things they can do to help with recovery, and emotional response to the disease.
When asked about their preferences for information presentation about treatment success rates, 70% had ≥1 preferred methods. Most participants (88%) preferred presentation in percentages, 59% wanted to hear about a previous patient that the physician had treated, 37% preferred qualitative descriptions and 30% preferred presentation in fractions. Compared to younger adults, older adults were less likely to prefer presentation in percentages (82% vs. 91%, p=0.04).
Prognostic optimism occurred in 31% (Figure 1b). On multivariate analysis, only older age was associated with prognostic optimism (OR 1.05, p=0.03).
Conclusions:
Our study suggests that decisional involvement and information preferences vary among patients with hematologic malignancies and should be assessed explicitly as part of each decision-making encounter to ensure patients' needs are being met. In addition, approximately one-third of patients had prognostic optimism. Although most studies find that physicians follow the same script with their patients and present invariant information, given the heterogeneity of patient preferences, physicians need to tailor their encounters.
Loh:Seattle Genetics: Consultancy; Pfizer: Consultancy. Leblanc:Agios, AbbVie, and Bristol Myers Squibb/Celgene: Speakers Bureau; UpToDate: Patents & Royalties: Royalties; American Cancer Society, BMS, Duke University, NINR/NIH, Jazz Pharmaceuticals, Seattle Genetics: Research Funding; AbbVie, Agios, Amgen, AstraZeneca, CareVive, BMS/Celgene, Daiichi-Sankyo, Flatiron, Helsinn, Heron, Otsuka, Medtronic, Pfizer, Seattle Genetics, Welvie: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees; AstraZeneca: Research Funding. Lee:Pfizer: Consultancy, Research Funding; Incyte: Consultancy, Research Funding; AstraZeneca: Research Funding; Kadmon: Research Funding; Novartis: Research Funding; Takeda: Research Funding; Syndax: Research Funding; Amgen: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal